670 Case Study Psychiatric SOAP Note Solved Template with Rx – Best Nursing Assignment Solutions
This article covers a solution to 670 Case Study Psychiatric SOAP Note Template with Rx assignment.
Permalink: https://customnursingassignments.com/case-study-psychiatric-soap-note
customnursingassignments.com has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us.(Case Study Psychiatric SOAP Note)
670 Case Study Psychiatric SOAP Note Template with Rx
There are different ways in which to complete a Psychiatric SOAP (Subjective, Objective, Assessment, and Plan) Note. This is a template that is meant to guide you as you continue to develop your style of SOAP in the psychiatric practice setting.
| Criteria | Clinical Notes |
| Subjective Include chief complaint, subjective information from the patient, names and relations of others present in the interview, and basic demographic information of the patient. HPI, Past Medical and Psychiatric History, Social History. | Chief Complaint- Patient (John) says he seeks consultation because he has some legal issues regarding drinking and driving that he thinks were likely fueled by his psychiatric symptoms. The college graduate is currently euthymic has never had suicidal ideation but some of the depressive episodes have incapacitated and interfered with both school and work. HPI- Just before the manic episodes a few months ago John was started on a selective serotonin reuptake inhibitor (SSRI) for SAD (Seasonal Affective Disorder) symptoms as well as depression. Within days of initiation of SSRI medication he experience elevated mood. In addition to having episodes of low self-esteem, rejection sensitive and guilt ridden for no reason he reports social anxiety symptoms and is often nervous around new people and acquaintances. Due to anticipatory anxiety experiences, he opts to avoid certain social events as the symptoms manifest independent of his affective state. The SSRI medication made him lose anxiety, fear and avoidance. He reports that the mood elevation abated after SSRI cessation. Past Medical and Psychiatric History- The patient though currently euthymic has a history of major depressive episodes most of which were untreated since his adolescence. He is not on any medication currently. The symptoms have varied in severity and length manifesting as insomnia, depressed mood, and low interest in activities, poor energy and despondent thoughts. Family History– No family history of bipolar disorder; Mother has generalized anxiety disorder (GAD) Social History- Upon graduation, the 26-year-old reports having a few friends and very supportive family. He wants to be a news reporter. |
| Objective This is where the “facts” are located. Include relevant labs, test results, vitals, and Review of Systems (ROS) – if ROS is negative, “ROS noncontributory,” or “ROS negative with the exception of…” Include MSE, risk assessment here, and psychiatric screening measure results. | Labs, test results- A thyroid function test to measure the patient’s thyroid gland functions. This would help rule out hypothyroidism another cause for depressive symptoms. Vitamin D: To rule out Vit D deficiency which insufficiency may contribute to depression and other mental illness. Kidney and Liver function test: Will use this panel to evaluate if both organs are functioning proper as they are responsible for eliminating antipsychotic and anti-depressant medication from the body. Vitals- 98.8, 160/80, 76, 18, 5’10”, and 190 lbs Review of Systems (ROS) – Patient reports mood swings from low self- esteem to guilt ridden and fear of rejection for no apparent reason. He is also affirmative of insomnia, increased energy and elevated moods when on SSRIs. Other manic symptoms were; Patient denies suicidal ideation, grandiosity exhibition, felt he was invincible and that he was above the law. These feelings made him pick a quarrel with a man in a bar, drove under the influence and challenge the authority when the police intervened. MSE I. Appearance: Stated age II. Behavior: Engaged III. Attitude: Easily distracted IV. Level of Consciousness: Alert V. Orientation: Impaired cognition VI. Speech and Language: Talkative, clear VII. Mood: depressed, low energy, hyperactive VIII. Affect: Sad, euthymic and anxious IX. Thought Process/Form: Sensitive, racing thought, goal directed X. Thought Content: Sad, angry, detached from others, impulsive, grandiose. XI. Suicidality and Homicidality: No suicidal or homicidal thought XII. Insight and Judgment: Aware of condition XIII. Attention Span: Easily distracted XIV. Memory: Impaired XV. Intellectual Functioning Mini Mental State Examination (MMSE): 30/30 Alcohol Use Disorders Identification Test (AUDIT): 3 Generalized Anxiety Disorder (GAD-7): 5 Psychiatric screening measure results– The psychiatric screening results report normal function of Thyroid stimulating Hormone; LFT; Vit D and Kidney function panel. |
| Assessment Include your findings, diagnosis and differentials (DSM-5 and any other medical diagnosis) along with ICD-10 codes, treatment options, and patient input regarding treatment options (if possible), including obstacles to treatment. | Findings- Normal thyroid gland, Vit D, LFT, and kidney function functioning established and mood charting indicative of episodes of mania, depressive episodes and anxiety. DSM-5 along with ICD-10 codes- The patient exhibiting Bipolar II disorder 296.89 (F31.81) (Active). This is determined since the BD symptoms does not interrupt the patient’s ability to function, there’s definitive major depression and anxiety. Depressive disorder due to another medical condition, with major depressive-like episode (F06.32) (Active). John seems to have met at least 5 of the 9 symptoms in the DSM V diagnostic criteria for Major Depressive Disorder, has been depressed more than once and been treated in the past. Differentials: Major Depressive Disorder, Severe with Psychotic Features (F33.3): This appears possible due to depressive statements from patient with reports of low esteem, decreased energy, insomnia and previous hx of depression. Substance-Related Disorders or Alcohol induced disorders (F10.99): Ruled out at this time from patient’s AUDIT screening with score of 3 (low risk) which occurred during college times on weekend only. Social Anxiety Disorder (F41.1): This seems quite possible from GAD-7 screening as patient scored 5. It appears that the symptoms have been present through most of his life and college and have not developed along with any one specific medical condition. Treatment options- Whether depressive, dysthymic, and mixed states constitute the majority of BD illness burden. Recommendation for patient is to be placed treatment regimen of antidepressants, mood stabilizers such as carbamazepine for short term and lamotrigine and second-generation antipsychotics. The patient’s input is to engage in non-pharmacological interventions like psychotherapy. The obstacles to treatment include failure of the patient to adhere to the prescribed medication and his lack of knowledge on management and treatment options for BD. |
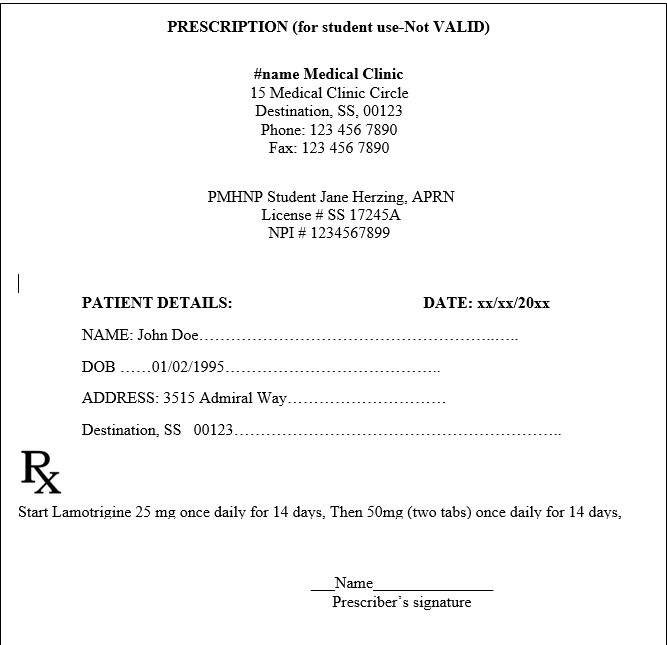
| Plan Include a specific plan, including medications & dosing & titration considerations, lab work ordered, referrals to psychiatric and medical providers, therapy recommendations, holistic options and complimentary therapies, and rationale for your decisions. Include when you will want to see the patient next. This comprehensive plan should relate directly to your Assessment. | Plan to start Lamotrigine at 25 mg once daily for 2 weeks, titrate then to 50mg once daily for 2 weeks, then 100mg once daily for one week. Plan to schedule a follow up appt with patient on or during the initiation of the 50mg schedule. Patient to obtain creatinine level and electrolytes to ensure adequate kidney function to be able to excrete the medications from the body and to ensure the kidney can handle the medication if titration occurs. Will educate patient to continue to keep daily record of moods and sleep patterns as this will assist to evaluate the treatment is adequate for john and achieving a good therapeutic range. Will refer to mental health psychiatrist for confirmation of diagnosis. Will refer to the primary care physician to evaluate the mildly elevated blood pressure. Will refer to psychotherapies such as (cognitive-behavioral therapy, family focused therapy, interpersonal and social rhythm therapy) to improve both symptoms, behavior and functioning. Will recommend multivitamins that will include omega 3, Vitamin B, D, B12 and folate. As these vitamins are very essential for the functioning of neurons. Study by Ravindran et al. (2016) showed the vitamins helps to improve treatment of depression and other mood disorders. Daily exercise helps to maintain good physical and mental health. Acupuncture showed significant effective improvement after the treatment for patients with depression (Ravindran et al., 2016). Plan to proceed to maintenance dosing of Lamotrigine 200mg daily after obtaining baseline creatinine level if symptoms and behavior improved. The medication will be reinforced with continued outpatient counselling. This will reinforce to explore options, develop adequate strategies for John to increase his self-esteem. Follow up is set in 2 weeks or earlier if any depressive or mood behavior occurs or worsens. If no further improvement is noted after the four weeks or mania occurs prior to the follow up appt, will add Lithium or Olanzapine depending on the symptoms. |
Copy any Case study questions from the instructions and answer here.
- Does the patient’s history support a diagnosis of bipolar disorder even though his symptoms appear to have been triggered by a selective serotonin reuptake inhibitor?
As you continue, customnursingassignments.com has the top and most qualified writers to help with any of your assignments. All you need to do is place an order with us. (Case Study Psychiatric SOAP Note)

Yes, the patient’s history supports a bipolar diagnosis even before his manic symptoms became ‘full blown’ after he was placed on SSRIs. Anyayo et al. (2021) mentioned that mental health experts admit that diagnosis bipolar disorder is not an easy task there aren’t lab tests to make a confirmatory diagnosis and its correct diagnosis has to rely on a combination of methods, symptoms and behaviors.
Prior to initiating patient on the SSRIs, the 26-year man was having depressive episodes impaired cognition, despondent thoughts, depressed mood and poor energy among others. For the bipolar disorder before diagnosis to have manifested- the mania phase may have presented itself as recovery from the depression phase.
This diagnosis for bipolar disorder is made after ruling out other conditions where a thyroid function test is needed to rule out hypothyroidism, hypercalcemia, or other nutritional deficiencies. To diagnose bipolar disorder the patient must have at least one depression episode and one manic or hypomanic episode after a mental health evaluation (Anyayo et al., 2021).
- What would be the expected future course of illness for this patient?
Baldessarini, et al. (2020) identified in mental health evidence indicating that almost 50% of all Bipolar disorder diagnosed cases outgrow the condition between the ages of 18 and 25 years. However, since patient is already 26 years old one can expect the future course of the illness for the young man is the manic- Bipolar depression phases will continue to cause severe and unusual mood shifts and energy that significantly impact on the patients to execute his daily tasks.
Be that as it may, ongoing treatment and self-management can see the patient maintain stable moods for long periods of time.
- If the patient develops another depressive episode, how would you treat it?
To treat another depressive episode, I would use lamotrigine as it reduces the risk of depressive episodes recurrences on a long term basis. Adjunct of Quetiapine or Valproate may substitute.
- What medication would you choose (there could be many correct answers).
FDA has approved Lamotrigine for long term prophylaxis in BD. Other medications that could be used is lithium or even second generation antipsychotics like quetiapine, lurasidone, olanzapine – fluoxetine and carbamazepine for short term treatment of BD acute depressive episodes (Gitlin, 2018). Taking Lamotrigine, despite its mechanism of action being not adequately understood, it belongs to the triazine group meaning that it selectively binds sodium channels.
The binding then stabilizes the presynaptic neuronal membrane and therefore inhibits the release of glutamate. Lamotrigine is also believed to impact other neurotransmitters like dopamine, serotonin and norepinephrine. Another theory contends that Lamotrigine has the capacity to interact with voltage activated calcium gated channels triggering a wide range of activity.
- Provide and reference a recent research article (Published over the last 3 years) on the medication treatment of Mood Disorders
Anyayo, L., Ashaba, S., Kaggwa, M.M., Maling, S. & Mpungu, E. (2021). Health-related quality of life among patients with bipolar disorder in rural southwestern Uganda: a hospital based cross sectional study. Health Qual Life Outcomes 19,84 (2021). https://doi.org/10.1186/s12955-021-01729-5
Baldessarini, R. J., Vázquez, G. H., & Tondo, L. (2020). Bipolar depression: a major unsolved challenge. International journal of bipolar disorders, 8(1), 1-13
Gitlin, M. J. (2018). Antidepressants in bipolar depression: an enduring controversy. International journal of bipolar disorders, 6(1), 1-7.
Ravindran, A.V., Balneaves, L.G., Faulkner, G., Ortiz, A., McIntosh, D., Morehouse, R.L., Ravindran, L., Yatham, L.N., Kennedy, S.H., Lam, R.W., MacQueen, G.M., Milev, R.V. & Parikh, S.V. (2016). Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 Clinical Guidelines for the Management of Adults with Major Depressive Disorder: Section 5. Complementary and Alternative Medicine Treatments. Canadian Journal of Psychiatry. Sep;61(9):576-87. doi: 10.1177/0706743716660290.
